- [email protected]
- +44 (0) 23 8048 3000
Getting a FIT Sample
- Resource: Reports
- Date: November 2, 2017
Improve Sample Integrity for Faecal Haemoglobin
One of the challenges in clinical diagnostics is the logistics of getting a quality sample from the patient to the laboratory for analysis.
When considering the detection of faecal haemoglobin (f-Hb), this is partly dependent on the technology to be employed. In the days of guaiac based faecal testing, samples were sent in traditional blue-capped “stool pots”. This was clearly wrong, since haemoglobin in native faeces is very unstable (Brown and Fraser1). It degrades rapidly at physiological and ambient temperatures. In passed faeces which contain digestive enzymes, bacteria and fungi, it will degrade even faster.
The moiety being examined in gFOBT is the haem component of the haemoglobin molecule. Young et al.2 demonstrated that, with gFOBT, the degradation was more pronounced in the samples that were not dried, as when collected into a traditional faecal pot, versus a thin dried smeared sample (taken directly onto the gFOBT card). The conclusion was that sampling directly onto the card should be made as soon as possible following defecation. In addition, analysis of gFOBT should be delayed for a few days so that potential interference from plant peroxidases, leading to false positive results, can be minimised.3
With the move to a more sensitive technology based on an immunoassay specific for human haemoglobin, it is vital to stabilise the haemoglobin present in the specimen collection device, prior to analysis, to protect it from degradation and maintain integrity.
Brown and Fraser1 performed a similar study to Young et al2. However, they used both qualitative and quantitative FIT methods to analyse five haemoglobin spiked faecal samples, with daily sampling for up to 14 days. The conclusion was that false negative results for faecal haemoglobin could occur if sampling fresh into the tubes or onto the cards of FIT collection devices is delayed.
With the release NICE Guidance DG30, now focussing on the benefits of the application of FIT as a means to triage patients with lower gastrointestinal (GI) symptoms, it is important that any loss of f-Hb is protected.
Using a low level cut-off of 10μg of Hb/ g faeces, the negative predictive value (NPV) for cancer is very high (100 % in the hallmark study by McDonald et al.4). Similarly high NPVs of 94%, are seen for higher risk adenomas (HRA) and Inflammatory Bowel Disease (IBD). Further studies in the UK have also shown a high degree of NPV when using FIT with cut-offs at this f-Hb concentration.5,6,7
The introduction of new quantitative FIT methods has vastly improved the method of faecal sample collection.
This is an important aspect of the process since the clinical outcomes are dependent on the ability of the method to detect faecal haemoglobin at very low versus undetectable concentrations.
The HM-JACKarc specimen collection device contains a proprietary buffer which can stabilise f-Hb in samples
for up to 14 days at ambient temperature (up to 25 °C) or up to 120 days in the fridge (4°C). This was confirmed in a study by Carroll et al.8 investigating the performance characteristics of four FIT methods.7
With any method, sample integrity is key to the quality of result and the pre-analytical component is key.
Sample size and consistency have always been an issue with faecal testing. Typically laboratories would be concerned that a layperson would be unable to provide a consistent sample. However, with the specifically designed collection device for the HM-JACKarc, this is made easier for those taking the sample, irrespective of whether that is the laboratory professional or the patient.
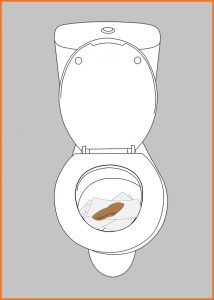
The unique HM-JACKarc sample collection probe has two hexagonal dimples on one side. When this is placed back into the collection tube, after sampling of the faeces, any excess faecal matter is removed as the probe passes through the hexagonal hole and rubber septum. This ensures that a consistent amount of faecal sample is passed into the constant volume of buffer, irrespective of the consistency of the faeces which can vary from liquid to hard pellets. The HM-JACKarc sample device also contains a proprietary buffer that immediately stabilises the f-Hb.
Use of the HM-JACKarc specimen collection device ensures stability of f-Hb and low variation in the ratio of faecal mass collected to volume of buffer.
In addition the sampling device is much more acceptable for patients to use since they find it easier and more hygienic than the traditional guaiac cards which required two samples of faeces to be smeared onto the card on three occasions. The FIT sample only needs to be taken once and is quick and simple so it addresses the issues of those who have concerns about handling faeces, encouraging more to take the test.
Pilot studies have shown an increased uptake in screening programmes and it is estimated that adopting FIT will increase screening uptake by around 10%. This would mean an additional 200,000 people could be tested each year.
Results of a 6-month FIT pilot9 involving 39,460 patients showed almost double the uptake with FIT than with gFOBt for previous non-responders (up from 14.5% to 26.6%).
There was an increase in participation for those invited for the first time, from 50.2% to 61.5% and also for those who had participated previously (from 86.6% to 91.1%).
Of particular note is the increase in uptake in the traditionally ‘hard to reach’ deprived population, which was up from 46.9% to 55.1%.
References
- Brown LF, Fraser CG. Effect of delay in sampling on haemoglobin determined by faecal immunochemical tests. Ann Clin Biochem. 2008;45:604-5.
- Young GP, Sinatra MA, St John DJ. Influence of delay in stool sampling on fecal occult blood test sensitivity. Clin Chem. 1996;42:1107-8.
- Sinatra MA, St John DJ, Young GP. Interference of plant peroxidases with guaiac-based fecal occult blood tests is avoidable. Clin Chem. 1999;45:123-6.
- McDonald PJ, Digby J, Innes C, et al. Low faecal haemoglobin concentration potentially rules out significant colorectal disease. Colorectal Dis. 2013;15:e151-9.
- Mowat C, et al. Faecal haemoglobin and faecal calprotectin as indicators of bowel disease in patients presenting to primary care with bowel symptoms. Gut. 2016;65:1463-9.
- Godber IM, et al. Use of a faecal immunochemical test for haemoglobin can aid in the investigation of patients with lower abdominal symptoms. Clin Chem Lab Med. 2016;54:595-602.
- Thomas CL, et al. Can immunochemical tests for faecal haemoglobin and faecal calprotectin be used to risk stratify patients for referral to colonoscopy for suspected colorectal cancer? Ann Clin Biochem. Biochemistry 2016;53 Suppl 1:38-9.
- Carroll MR, Seaman HE, Halloran SP Tests and investigations for colorectal cancer screening. Clin Biochem. 2014;47:921-39
- Moss S et al. Increased uptake and improved outcomes of bowel cancer screening with a faecal immunochemical test: results from a pilot study within the national screening programme in England. Gut.2017 Sep;66(9):1631-1644. doi: 10.1136/gutjnl-2015-310691. Epub 2016 Jun 7.